
2019 benets at a glance
independence choice
WORKFORCE OPTIMIZATION
®
Benefits at a glance .......................................................................1
Medical coverage map ....................................................................3
Medical coverage terms ...................................................................4
Medical coverage options .................................................................6
Dental benefits at a glance ................................................................8
Vision benefits at a glance .................................................................9
This brochure provides an overview of your Insperity benefits package. Actual benefits are subject to the provisions and
limitations of the agreements between Insperity and its benefits providers. Detailed benefits information is available on the
Insperity Premier
™
platform at portal.insperity.com.
Except where otherwise indicated, employees must be generally working 30 or more hours per week, on average (20 hours
per week in Hawaii), or meet the requirements for continuing eligibility during an approved leave of absence, to be eligible
for the health and welfare benefits in this package. Certain individuals are excluded from participation in Insperity Plans.
Please refer to the Summary Plan Description (SPD) for each Plan on Insperity Premier for full eligibility requirements.

portal.insperity.com 1 866.715.3552
The following benefits are available to full-time (or full-time equivalent) Insperity employees that generally work 30 or more
hours per week (20 or more hours in Hawaii) on average, and meet all other eligibility requirements:
The Insperity Group Health Plan
Medical coverage options include prescription coverage and vary by insurance carrier, region and coverage type.
All coverage options also generally include wellness programs and telemedicine options (where permied by state law).
Availability is determined by benefits package and ZIP code service area. Dental and vision coverage is available through
UnitedHealthcare Dental and Vision Service Plan nationwide, and may be elected independently of medical coverage.
The Insperity Health Care Flexible Spending Account (FSA) Plan
Make pretax contributions (if eligible) up to the annual maximum through payroll deduction for qualifying health care
expenses incurred during the plan year.
The Insperity Health Savings Account (HSA) Program
If enrolled in an Insperity High Deductible Health Plan (HDHP) option, make contributions by payroll deduction on a pretax
basis (if eligible) or on a post-tax basis up to established annual federal limits for qualifying health care expenses.
The Insperity Welfare Benefits Plan
Benefits include employer-paid basic term life and personal accident insurance equal to 1 x covered annual earnings
($50,000 maximum). Disability coverage for up to 60% of covered weekly or monthly earnings is available to you as a
voluntary (employee-paid) benefit. Voluntary life and personal accident insurance is also available to you and your eligible
dependents. See the Voluntary Benefits Book for coverage amounts and rates.
The Insperity Adoption Assistance Program
Reimburses up to $1,500 of qualifying expenses per qualified adoption. Requires 180 days of continuous service aer
obtaining eligible status.
Benets at a glance
Life, Personal Accident and Disability Coverage Amounts
Coverage amounts for benefits are determined by your covered annual earnings, which include base or estimated
annual earnings plus amounts received as commissions, piece work and fee-based pay as paid by Insperity.

2
The following benefits are available to all Insperity employees, whether full-time, part-time or seasonal:
The Insperity Employee Assistance Program
A counseling and consultation service available to all employees (and their dependents) with no hourly eligibility
requirement. Most services are available at no cost.
The Insperity Commuter Benefits Program
Pay for job-related mass transit and/or parking expenses with pretax dollars (if eligible).
Learning and Development
Self-paced online, live virtual and classroom training programs to learn new skills, maintain safety and compliance, improve
performance and develop careers.
Insperity Pay Options
Payroll direct deposit and debit pay card options are available.
MarketPlace
™
Offers online discounts on a variety of goods and services, including identity the protection, pet health insurance, travel,
electronics, gis, household needs and more.
Benets at a glance
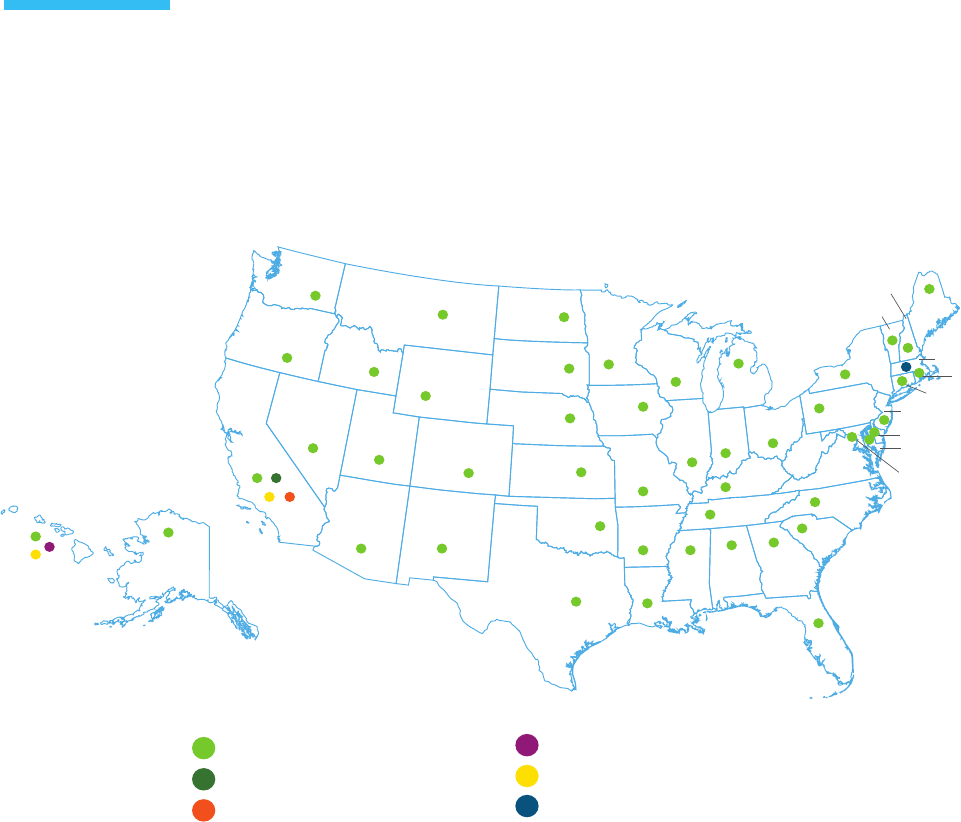
WA
OR
CA
NV
UT
AZ NM
CO
WY
SD
NE
KS
OK
TX
AK
HI
ID
MT
ND
MN
MI
IN
OH
WV
VA
PA
NY
VT
NH
ME
MA
RI
CT
NJ
DE
MD
DC
WI
IL
IA
MO
KY
TN
MS
AL
GA
SC
NC
FL
AR
LA
Tus
Kaiser Permanente
HMSA BlueCross BlueShield of Hawaii
UnitedHealthcare
UnitedHealthcare of California
Blue Shield of California
portal.insperity.com 3 866.715.3552
To participate in a coverage option, an eligible employee must live in a ZIP code service area included in that insurance
carrier’s network. ZIP codes associated with an insurance carrier’s network service area are determined by the insurance
carrier (not Insperity) and are specific to the health insurance product offerings defined in the carrier’s contract
with Insperity.
Where offered, an indemnity (out-of-area) option is available to employees who live in a ZIP code service area not served by
any Insperity insurance carrier’s network.
The Insperity Group Health Plan medical coverage options available to an eligible employee are determined by:
• The Insperity benefits package selected by the client company,
• The employee’s residential ZIP code service area, and
• The insurance carrier(s) and networks available in that area.
Medical coverage map

portal.insperity.com 4 866.715.3552
Calendar-year deductible
This is the amount owed for certain covered health care services before the plan begins to pay benefits. Not all covered
services require this deductible to be met (e.g., office visit copays under non-HDHP coverage options).
Except as otherwise noted for certain HDHP-type coverage options, Insperity coverage options generally have
“embedded” calendar-year deductibles and out-of-pocket maximums (OOPMs). For family coverage under the embedded
design, each covered family member needs to satisfy only an individual calendar-year deductible (not the entire family
deductible), before the individual member can receive covered medical services or prescription drugs at copay or
coinsurance levels. Individual family members are responsible for their own out-of-pocket covered medical expenses up to
the individual-level OOPM. Combined individual out-of-pocket covered medical expenses for a family will never exceed the
family-level OOPM.
Certain Insperity HDHP coverage options have “aggregate” (non-embedded) deductibles and OOPMs. For family coverage
under the aggregate design, the entire family calendar-year deductible must be met before copays or coinsurance will
apply for any individual family member. Only aer the full family deductible is met will any family member be able to receive
covered medical services or prescription drugs at copay or coinsurance levels. A family is responsible for all its members’
out-of-pocket covered medical expenses up to the family-level OOPM.
All Insperity coverage options cover in-network physician office visits for preventive care services (as defined in the
applicable Certificate of Coverage) at 100% with no copay or coinsurance, regardless of whether any deductible has
been met.
Annual out-of-pocket maximum (OOPM)
This is the most a participant must pay out of their own pocket during the calendar year before the plan begins to pay 100%
of eligible expenses. Medical calendar-year deductibles, copays and coinsurance (including prescriptions, unless otherwise
noted) generally apply toward satisfying the annual out-of-pocket maximum. Insperity coverage options with embedded
deductibles will have embedded OOPMs; HDHP coverage options with aggregate deductibles will have aggregate OOPMs.
Medical coverage terms

portal.insperity.com 5 866.715.3552
Copays
A fixed amount you pay for a covered service from an in-network provider. Generally, whenever a medical copay applies,
coinsurance will not apply, and you are not required to first satisfy any applicable medical calendar-year deductible.
Coinsurance
This is your share of the cost of a covered service, calculated as a percent of the allowed amount for the service. Coinsurance
(where applicable) applies aer the participant satisfies any applicable calendar-year deductible. Also, coinsurance generally
will not apply where a copay applies.
In-network
Providers and facilities that contract with your health insurance carrier are considered in-network; you will pay in-network
copays, deductibles and coinsurance rates for eligible expenses from network providers.
Out-of-network
Providers and facilities that do not contract with your health insurance carrier are considered out-of-network.
If your coverage option does not include out-of-network coverage, no benefits will be paid for services received from
out-of-network providers, except for emergency medical treatment.
If your elected coverage option pays benefits for services received from out-of-network providers, your financial
responsibility will likely be much greater. It is important to understand how your specific insurance carrier reimburses for
out-of-network services, and it is your responsibility to pay any cost difference between what the out-of-network provider
charges and what the plan covers (i.e., what the insurance carrier pays). In addition, the cost difference, which could be
substantial depending on the cost of the care received, does not apply to the out-of-pocket maximum.
The plan year for the Insperity Group Health Plan is the calendar year.
Plan design changes take effect each Jan. 1, and may include increases to out-of-pocket costs such as copays,
coinsurance, annual deductibles and annual out-of-pocket maximums. Coverage periods under the Plan will
last 12 months, and will vary by client company based on the renewal date of the client company’s contract
with Insperity.
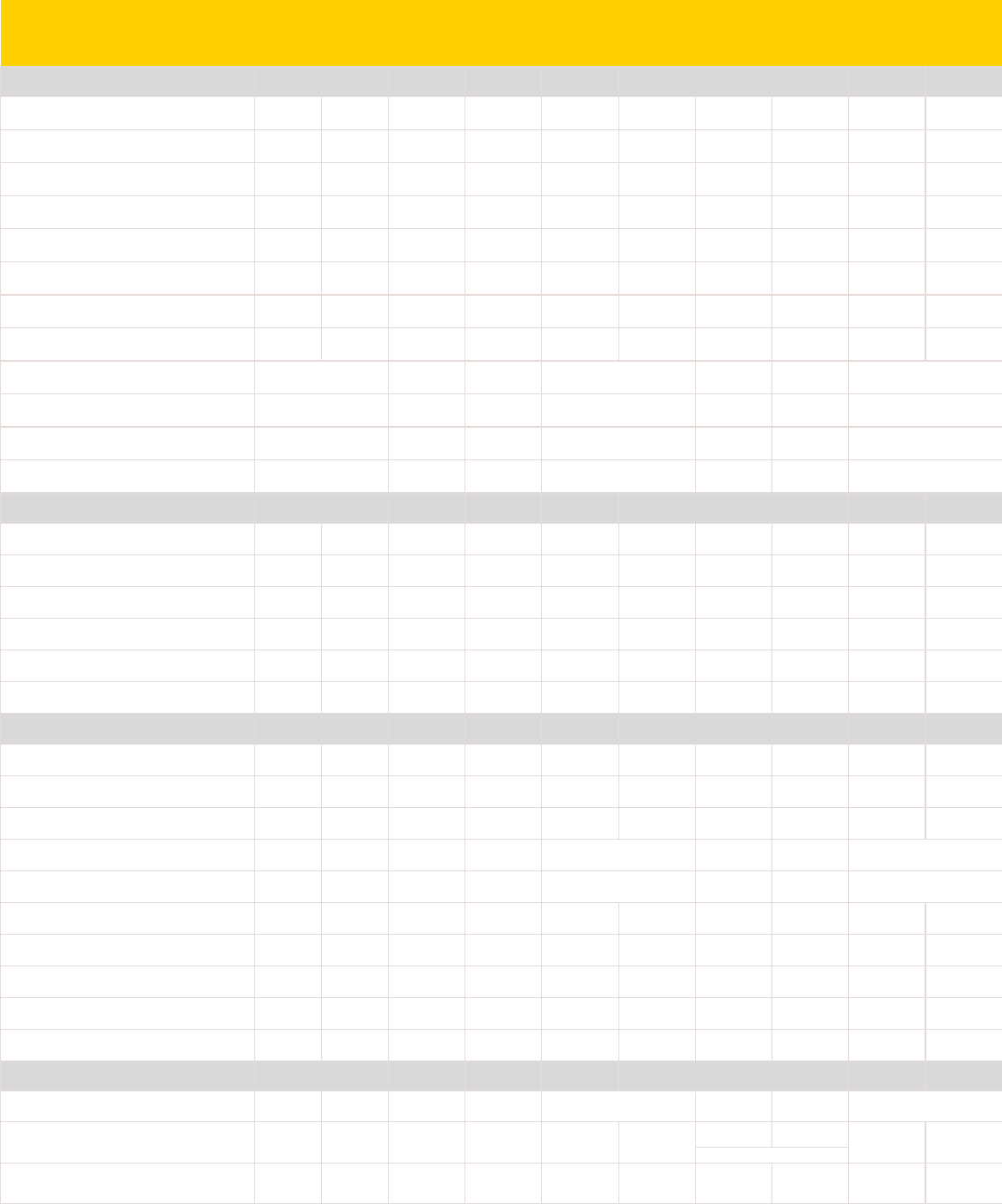
coverage options
by state physician specialist telemedicine outpatient
surgery
inpatient
hospital
urgent care
clinic
emergency
room
National
in-network
out-of-
network
in-network
individual
in-network
family
out-of-network
individual
out-of-network
family
in-network
individual
in-network
family
out-of-network
individual
out-of-network
family
office visit office visit virtual visit OPS IPH UC ER individual family tier 1 tier 2 tier 3 tier 4
UnitedHealthcare Choice Plus 500/80 80% 60% $500 $1,500 $1,000 $3,000 $5,000 $10,000 $10,000 $20,000 $35 $60 $20 20% 20% $75 $250 $100 $300 $10 $35 $60 $120
UnitedHealthcare Choice Plus 1000 80% 60% $1,000 $3,000 $2,000 $6,000 $4,500 $9,000 $9,000 $18,000 $35 $60 $20 20% 20% $75 $250 $100 $300 $10 $35 $60 $120
UnitedHealthcare Choice Plus 1500 80% 60% $1,500 $4,500 $3,000 $9,000 $6,350 $12,700 $12,700 $25,400 $35 $60 $20 20% 20% $75 $250 $100 $300 $10 $35 $60 $120
UnitedHealthcare Choice Plus 2500 70% 50% $2,500 $7,500 $5,000 $15,000 $6,850 $13,700 $13,700 $27,400 $40 $70 $20 30% 30% $75 $250 $100 $300 $10 $35 $60 $120
UnitedHealthcare Choice Plus 6000 100% 70% $6,000 $13,200 $12,000 $16,400 $7,000 $14,000 $14,000 $28,000 $40 $70 $20 0% 0% $75 $500 $200 $600 $10 $35 $60 $120
UnitedHealthcare Choice Plus HDHP 1500
aggregate deductible option
90% 70% $1,500 $3,000 $3,000 $6,000 $4,000 $7,350 $8,000 $14,700 10% 10% 10% 10% 10% 10% 10% $10 $35 $60 $120
UnitedHealthcare Choice Plus HDHP 3000 90% 70% $3,000 $6,000 $6,000 $12,000 $6,650 $13,300 $13,300 $26,600 10% 10% 10% 10% 10% 10% 10% $10 $35 $60 $120
UnitedHealthcare Choice Plus HDHP 5000 80% 60% $5,000 $10,000 $10,000 $20,000 $6,650 $13,300 $13,300 $26,600 20% 20% 20% 20% 20% 20% 20% $10 $35 $60 $120
UnitedHealthcare Out-of-Area 500 $500 $1,500 $6,350 $12,700 20% 20% $20 20% 20% 20% 20% $100 $300 $10 $35 $60 $120
UnitedHealthcare Out-of-Area HDHP 1500
aggregate deductible option
$1,500 $3,000 $4,000 $7,350 20% 20% 20% 20% 20% 20% 20% $10 $35 $60 $120
UnitedHealthcare Out-of-Area HDHP 3000 $3,000 $6,000 $6,650 $13,300 20% 20% 20% 20% 20% 20% 20% $10 $35 $60 $120
UnitedHealthcare Out-of-Area HDHP 5000 $5,000 $10,000 $6,650 $13,300 20% 20% 20% 20% 20% 20% 20% $10 $35 $60 $120
California
(choose national or regional options)
in-network
out-of-
network
in-network
individual
in-network
family
out-of-network
individual
out-of-network
family
in-network
individual
in-network
family
out-of-network
individual
out-of-network
family
office visit office visit virtual visit OPS IPH UC ER individual family tier 1 tier 2 tier 3 tier 4
UnitedHealthcare of California HMO 100% n/a n/a n/a n/a n/a $3,000 $6,000 n/a n/a $25 $50 $25 $125 $500 $25 $200 n/a n/a $10 $30 $50
specialty rx
30% max
$200
Blue Shield of California HMO 100% n/a n/a n/a n/a n/a $3,000 $6,000 n/a n/a $25 $50 $5 $150 $500 $25 $200 n/a n/a $10 $25 $40
specialty rx
30% max
$200
Blue Shield of California Deductible HMO 1000 90% n/a $1,000 $2,000 n/a n/a $6,050 $12,100 n/a n/a $35 $50 $5 10% 10% $35 10% $10 $30 n/a
specialty rx
30% max
$200
Kaiser Permanente HMO 100% n/a n/a n/a n/a n/a $3,000 $6,000 n/a n/a $25 $50 $0 $100 $250 $25 $200 n/a n/a $10 $30 n/a
specialty rx
30% max
$150
Kaiser Permanente Deductible HMO 1000 70% n/a $1,000 $2,000 n/a n/a $6,050 $12,100 n/a n/a $35 $50 $0 30% 30% $35 30% $10 $30 n/a
specialty rx
30% max
$150
Kaiser Permanente HMO HDHP 90% n/a $2,700 $5,400 n/a n/a $5,200 $10,400 n/a n/a 10% 10% 0% 10% 10% 10% 10% $10 $30 n/a
specialty rx
30% max
$150
Massachusetts
(choose regional options only)
in-network
out-of-
network
in-network
individual
in-network
family
out-of-network
individual
out-of-network
family
in-network
individual
in-network
family
out-of-network
individual
out-of-network
family
office visit office visit virtual visit OPS IPH UC ER individual family tier 1 tier 2 tier 3 tier 4
Tufts CareLink Advantage PPO 500/80 80% 60% $500 $1,500 $1,000 $3,000 $5,000 $10,000 $10,000 $20,000 $35 $35 $35 20% 20% $35 $250 n/a n/a $10 $35 $60 n/a
Tufts CareLink Advantage PPO 1000 80% 60% $1,000 $3,000 $2,000 $6,000 $4,500 $9,000 $9,000 $18,000 $35 $35 $35 20% 20% $35 $250 n/a n/a $10 $35 $60 n/a
Tufts CareLink Advantage PPO 1500 80% 60% $1,500 $4,000 $3,000 $8,000 $6,350 $12,700 $10,000 $20,000 $35 $35 $35 20% 20% $35 $250 n/a n/a $10 $35 $60 n/a
Tufts CareLink Advantage Saver PPO HDHP 1500
aggregate deductible option
90% 70% $1,500 $3,000 $4,000 $7,350 10% 10% 10% 10% 10% 10% 10% $10 $35 $60 n/a
Tufts CareLink Advantage Saver PPO HDHP 3000
aggregate deductible option
90% 70% $3,000 $6,000 $4,000 $7,350 10% 10% 10% 10% 10% 10% 10% $10 $35 $60 n/a
Tufts Value HMO 100% n/a n/a n/a n/a n/a $3,000 $6,000 n/a n/a $25 $40 $25 $100 $500 $25 $250 n/a n/a $10 $30 $60 n/a
Tufts Advantage Deductible HMO 1000 100% n/a $1,000 $2,000 n/a n/a $5,000 $10,000 n/a n/a $25 $40 $25 0% 0% $25 $250 n/a n/a $15 $30 $60 n/a
Tufts Advantage Deductible HMO 2000 100% n/a $2,000 $4,000 n/a n/a $6,350 $12,700 n/a n/a $30 $45 $30 0% 0% $30 $250 n/a n/a $15 $30 $60 n/a
Tufts Advantage Saver HMO HDHP 1500
aggregate deductible option
90% n/a $1,500 $3,000 n/a n/a $4,000 $7,350 n/a n/a 10% 10% 10% 10% 10% 10% 10% $10 $35 $60 n/a
Tufts Advantage Saver HMO HDHP 3000
aggregate deductible option
65% n/a $3,000 $6,000 n/a n/a $4,000 $7,350 n/a n/a 35% 35% 35% 35% 35% 35% 35% $15 $30 $60 n/a
Hawaii
(choose regional options only)
in-network
out-of-
network
in-network
individual
in-network
family
out-of-network
individual
out-of-network
family
in-network
individual
in-network
family
out-of-network
individual
out-of-network
family
office visit office visit virtual visit OPS IPH UC ER individual family tier 1 tier 2 tier 3 tier 4
UnitedHealthcare Options PPO 90% 70% $100 $300 $2,500 $7,500 10% 10% $20 10% 10% 10% 10% $10 $15 $30 n/a
$2,500 $7,500
$3,600 $4,200
$10 $35 $35 $200
in-network copay or coinsurance for non-preventive care
the most you will pay before plan pays 100% amount owed before coinsurance applies after deductible
combined in/out of network
combined in/out of network
combined in/out of network
combined in/out of network
no network limitation
no network limitation
no network limitation
combined in/out of network combined in/out of network
medical only
$20n/a n/a $20 $20 $0 10%HMSA BlueCross BlueShield of Hawaii HMO n/a n/a n/a n/a90% n/a 10%
copays apply once medical deductible is met
$100 per member for brand drugs
retail prescription copay medical calendar-year deductible annual out-of-pocket maximum coinsurance prescription deductible
80%
80%
80%
80%
no network limitation
$100 per member for select drugs
no network limitation
no network limitation
no network limitation
no network limitation
n/a
applies to medical OOPM unless
otherwise noted
Kaiser Permanente HMO 100% n/a $20 $20 $20n/a n/a $6,000 n/an/a n/a $2,000 n/a $20 $50 per day $20 $50
Choice Plus and PPO coverage options have in- and out-of-network coverage. HMO coverage options have in-network coverage only. Out-of-Area options have no network limitation. Coverage options have embedded deductibles and OOPMs
unless otherwise noted. Additional limits and exclusions apply. See the Insurer Benefits Description for complete coverage details.
n/a
applies to medical OOPM unless
otherwise noted
copays apply once medical deductible is met
copays apply once medical deductible is met
copays apply once medical deductible is met
copays apply once medical deductible is met
copays apply once medical deductible is met
copays apply once medical deductible is met
$100|$200
$7 $30 $30 + 45
$3 maintenance (generic tier only)
$100
prescription-only OOPM
copays apply once medical deductible is met
copays apply once medical deductible is met
copays apply once medical deductible is met
copays apply once medical deductible is met
6
2019 choice medical coverage options at a glance
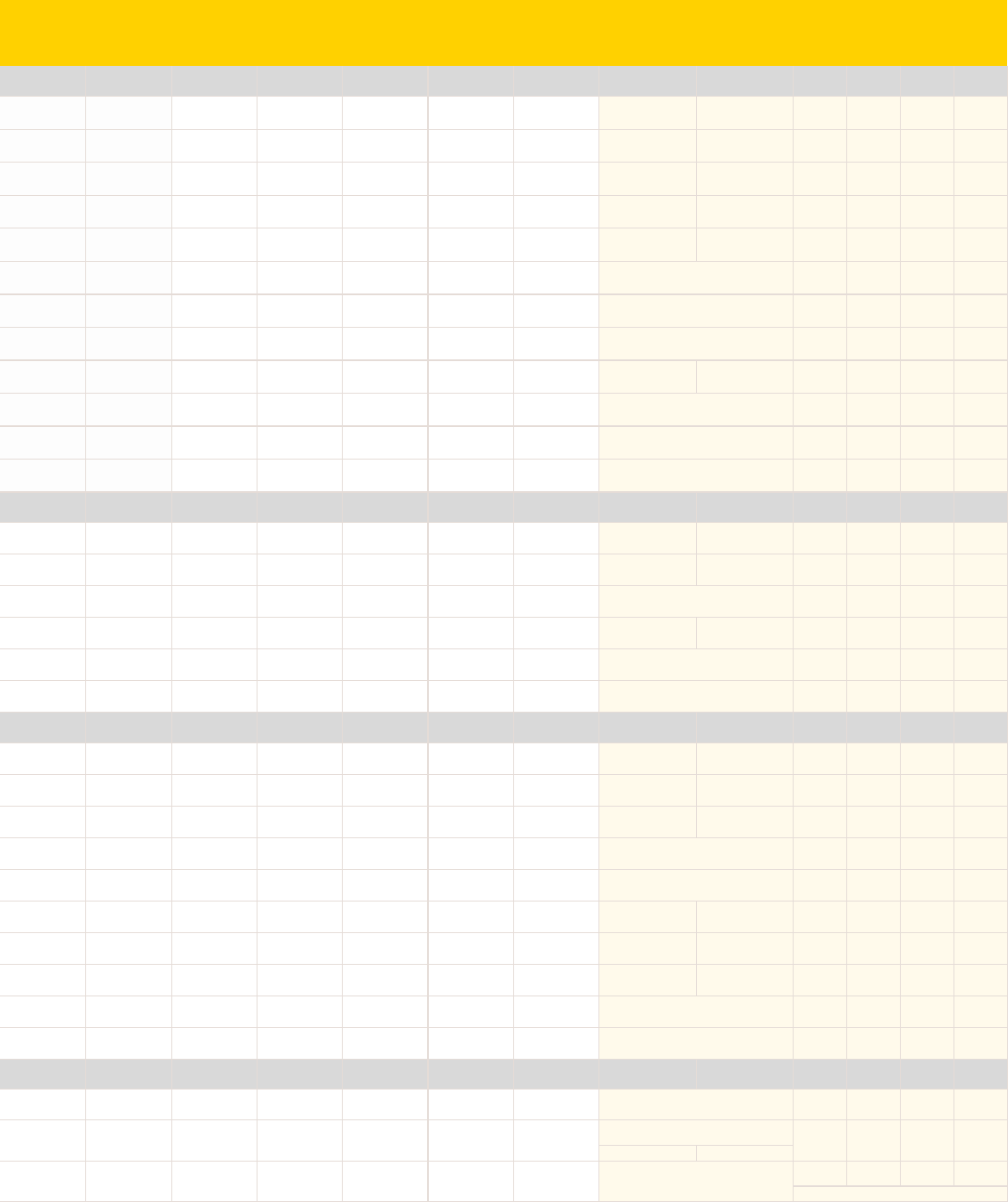
coverage options
by state physician specialist telemedicine outpatient
surgery
inpatient
hospital
urgent care
clinic
emergency
room
National
in-network
out-of-
network
in-network
individual
in-network
family
out-of-network
individual
out-of-network
family
in-network
individual
in-network
family
out-of-network
individual
out-of-network
family
office visit office visit virtual visit OPS IPH UC ER individual family tier 1 tier 2 tier 3 tier 4
UnitedHealthcare Choice Plus 500/80 80% 60% $500 $1,500 $1,000 $3,000 $5,000 $10,000 $10,000 $20,000 $35 $60 $20 20% 20% $75 $250 $100 $300 $10 $35 $60 $120
UnitedHealthcare Choice Plus 1000 80% 60% $1,000 $3,000 $2,000 $6,000 $4,500 $9,000 $9,000 $18,000 $35 $60 $20 20% 20% $75 $250 $100 $300 $10 $35 $60 $120
UnitedHealthcare Choice Plus 1500 80% 60% $1,500 $4,500 $3,000 $9,000 $6,350 $12,700 $12,700 $25,400 $35 $60 $20 20% 20% $75 $250 $100 $300 $10 $35 $60 $120
UnitedHealthcare Choice Plus 2500 70% 50% $2,500 $7,500 $5,000 $15,000 $6,850 $13,700 $13,700 $27,400 $40 $70 $20 30% 30% $75 $250 $100 $300 $10 $35 $60 $120
UnitedHealthcare Choice Plus 6000 100% 70% $6,000 $13,200 $12,000 $16,400 $7,000 $14,000 $14,000 $28,000 $40 $70 $20 0% 0% $75 $500 $200 $600 $10 $35 $60 $120
UnitedHealthcare Choice Plus HDHP 1500
aggregate deductible option
90% 70% $1,500 $3,000 $3,000 $6,000 $4,000 $7,350 $8,000 $14,700 10% 10% 10% 10% 10% 10% 10% $10 $35 $60 $120
UnitedHealthcare Choice Plus HDHP 3000 90% 70% $3,000 $6,000 $6,000 $12,000 $6,650 $13,300 $13,300 $26,600 10% 10% 10% 10% 10% 10% 10% $10 $35 $60 $120
UnitedHealthcare Choice Plus HDHP 5000 80% 60% $5,000 $10,000 $10,000 $20,000 $6,650 $13,300 $13,300 $26,600 20% 20% 20% 20% 20% 20% 20% $10 $35 $60 $120
UnitedHealthcare Out-of-Area 500 $500 $1,500 $6,350 $12,700 20% 20% $20 20% 20% 20% 20% $100 $300 $10 $35 $60 $120
UnitedHealthcare Out-of-Area HDHP 1500
aggregate deductible option
$1,500 $3,000 $4,000 $7,350 20% 20% 20% 20% 20% 20% 20% $10 $35 $60 $120
UnitedHealthcare Out-of-Area HDHP 3000 $3,000 $6,000 $6,650 $13,300 20% 20% 20% 20% 20% 20% 20% $10 $35 $60 $120
UnitedHealthcare Out-of-Area HDHP 5000 $5,000 $10,000 $6,650 $13,300 20% 20% 20% 20% 20% 20% 20% $10 $35 $60 $120
California
(choose national or regional options)
in-network
out-of-
network
in-network
individual
in-network
family
out-of-network
individual
out-of-network
family
in-network
individual
in-network
family
out-of-network
individual
out-of-network
family
office visit office visit virtual visit OPS IPH UC ER individual family tier 1 tier 2 tier 3 tier 4
UnitedHealthcare of California HMO 100% n/a n/a n/a n/a n/a $3,000 $6,000 n/a n/a $25 $50 $25 $125 $500 $25 $200 n/a n/a $10 $30 $50
specialty rx
30% max
$200
Blue Shield of California HMO 100% n/a n/a n/a n/a n/a $3,000 $6,000 n/a n/a $25 $50 $5 $150 $500 $25 $200 n/a n/a $10 $25 $40
specialty rx
30% max
$200
Blue Shield of California Deductible HMO 1000 90% n/a $1,000 $2,000 n/a n/a $6,050 $12,100 n/a n/a $35 $50 $5 10% 10% $35 10% $10 $30 n/a
specialty rx
30% max
$200
Kaiser Permanente HMO 100% n/a n/a n/a n/a n/a $3,000 $6,000 n/a n/a $25 $50 $0 $100 $250 $25 $200 n/a n/a $10 $30 n/a
specialty rx
30% max
$150
Kaiser Permanente Deductible HMO 1000 70% n/a $1,000 $2,000 n/a n/a $6,050 $12,100 n/a n/a $35 $50 $0 30% 30% $35 30% $10 $30 n/a
specialty rx
30% max
$150
Kaiser Permanente HMO HDHP 90% n/a $2,700 $5,400 n/a n/a $5,200 $10,400 n/a n/a 10% 10% 0% 10% 10% 10% 10% $10 $30 n/a
specialty rx
30% max
$150
Massachusetts
(choose regional options only)
in-network
out-of-
network
in-network
individual
in-network
family
out-of-network
individual
out-of-network
family
in-network
individual
in-network
family
out-of-network
individual
out-of-network
family
office visit office visit virtual visit OPS IPH UC ER individual family tier 1 tier 2 tier 3 tier 4
Tufts CareLink Advantage PPO 500/80 80% 60% $500 $1,500 $1,000 $3,000 $5,000 $10,000 $10,000 $20,000 $35 $35 $35 20% 20% $35 $250 n/a n/a $10 $35 $60 n/a
Tufts CareLink Advantage PPO 1000 80% 60% $1,000 $3,000 $2,000 $6,000 $4,500 $9,000 $9,000 $18,000 $35 $35 $35 20% 20% $35 $250 n/a n/a $10 $35 $60 n/a
Tufts CareLink Advantage PPO 1500 80% 60% $1,500 $4,000 $3,000 $8,000 $6,350 $12,700 $10,000 $20,000 $35 $35 $35 20% 20% $35 $250 n/a n/a $10 $35 $60 n/a
Tufts CareLink Advantage Saver PPO HDHP 1500
aggregate deductible option
90% 70% $1,500 $3,000 $4,000 $7,350 10% 10% 10% 10% 10% 10% 10% $10 $35 $60 n/a
Tufts CareLink Advantage Saver PPO HDHP 3000
aggregate deductible option
90% 70% $3,000 $6,000 $4,000 $7,350 10% 10% 10% 10% 10% 10% 10% $10 $35 $60 n/a
Tufts Value HMO 100% n/a n/a n/a n/a n/a $3,000 $6,000 n/a n/a $25 $40 $25 $100 $500 $25 $250 n/a n/a $10 $30 $60 n/a
Tufts Advantage Deductible HMO 1000 100% n/a $1,000 $2,000 n/a n/a $5,000 $10,000 n/a n/a $25 $40 $25 0% 0% $25 $250 n/a n/a $15 $30 $60 n/a
Tufts Advantage Deductible HMO 2000 100% n/a $2,000 $4,000 n/a n/a $6,350 $12,700 n/a n/a $30 $45 $30 0% 0% $30 $250 n/a n/a $15 $30 $60 n/a
Tufts Advantage Saver HMO HDHP 1500
aggregate deductible option
90% n/a $1,500 $3,000 n/a n/a $4,000 $7,350 n/a n/a 10% 10% 10% 10% 10% 10% 10% $10 $35 $60 n/a
Tufts Advantage Saver HMO HDHP 3000
aggregate deductible option
65% n/a $3,000 $6,000 n/a n/a $4,000 $7,350 n/a n/a 35% 35% 35% 35% 35% 35% 35% $15 $30 $60 n/a
Hawaii
(choose regional options only)
in-network
out-of-
network
in-network
individual
in-network
family
out-of-network
individual
out-of-network
family
in-network
individual
in-network
family
out-of-network
individual
out-of-network
family
office visit office visit virtual visit OPS IPH UC ER individual family tier 1 tier 2 tier 3 tier 4
UnitedHealthcare Options PPO 90% 70% $100 $300 $2,500 $7,500 10% 10% $20 10% 10% 10% 10% $10 $15 $30 n/a
$2,500 $7,500
$3,600 $4,200
$10 $35 $35 $200
in-network copay or coinsurance for non-preventive care
the most you will pay before plan pays 100% amount owed before coinsurance applies after deductible
combined in/out of network
combined in/out of network
combined in/out of network
combined in/out of network
no network limitation
no network limitation
no network limitation
combined in/out of network combined in/out of network
medical only
$20n/a n/a $20 $20 $0 10%HMSA BlueCross BlueShield of Hawaii HMO n/a n/a n/a n/a90% n/a 10%
copays apply once medical deductible is met
$100 per member for brand drugs
retail prescription copay medical calendar-year deductible annual out-of-pocket maximum coinsurance prescription deductible
80%
80%
80%
80%
no network limitation
$100 per member for select drugs
no network limitation
no network limitation
no network limitation
no network limitation
n/a
applies to medical OOPM unless
otherwise noted
Kaiser Permanente HMO 100% n/a $20 $20 $20n/a n/a $6,000 n/an/a n/a $2,000 n/a $20 $50 per day $20 $50
Choice Plus and PPO coverage options have in- and out-of-network coverage. HMO coverage options have in-network coverage only. Out-of-Area options have no network limitation. Coverage options have embedded deductibles and OOPMs
unless otherwise noted. Additional limits and exclusions apply. See the Insurer Benefits Description for complete coverage details.
n/a
applies to medical OOPM unless
otherwise noted
copays apply once medical deductible is met
copays apply once medical deductible is met
copays apply once medical deductible is met
copays apply once medical deductible is met
copays apply once medical deductible is met
copays apply once medical deductible is met
$100|$200
$7 $30 $30 + 45
$3 maintenance (generic tier only)
$100
prescription-only OOPM
copays apply once medical deductible is met
copays apply once medical deductible is met
copays apply once medical deductible is met
copays apply once medical deductible is met
7
Dental benets at a glance
Insperity dental and vision benefits must be elected together, but may be elected independently of medical coverage.
Benefits are generally available to eligible employees nationwide (if included in Insperity benefits package).
Benefit levels shown below are in-network. Services received from non-network providers will be paid at reasonable and
customary rates, and the participant will be responsible for any remaining balance.
• Preventive and diagnostic services include routine exams, cleaning, topical application of fluoride, diagnostic cast,
bite-wing x-rays, sealants and space maintainers.
• Basic (restorative) services include extractions, fillings, oral surgery, palliative emergency treatment, apicoectomy,
occlusal guards, periodontic services, root canal therapy, and therapeutic pulpotomy.
• Major services include inlays, crowns, bridges, dentures, denture rebase or reline, repair of removable dentures,
re-cementing of crowns and bridges, and repairs to fixed bridges.
• Orthodontic services include braces, retainers, and other appliances that correct misalignments for dependent
children to age 19 only.
• There is no coverage for placement/replacement of dental implants, implant-supported crowns, implant-supporting
structures, abutments or prostheses.
Additional limits and exclusions apply; see the Insurer Benefits Description for complete coverage details.
ID cards are issued when enrollment is processed.
UnitedHealthcare Dental | myuhc.com | 877.816.3596
calendar-year
deductible
per person
calendar-year
maximum
per person
orthodontia
lifetime
maximum
preventative and
diagnostic
services
basic
services
major
services
orthodontic
services
$50
$150 max per family
$1500
per year
$1500
to age 19 only
plan pays 100%
no deductible
plan pays 80%
aer deductible
plan pays 50%
aer deductible
plan pays 50%
no deductible
portal.insperity.com 8 866.715.3552
Vision benets at a glance
Insperity dental and vision benefits must be elected together, but may be elected independently of medical coverage.
Benefits are generally available to eligible employees nationwide (if included in Insperity benefits package).
Benefit levels shown below are in-network. The plan generally pays 100% of eligible expenses aer copay when network
providers are used. Services from non-network providers must be paid at full cost by the participant at the time of service. A
claim may then be filed for reimbursement of eligible expenses up to the out-of-network benefit allowance.
• You may receive a benefit for either glasses (lenses and frames) or contact lenses per 12-month period, but not both.
• Diabetic Eyecare Program Plus provides medical exams for diabetic eye disease, glaucoma, and age-related macular
degeneration (AMD), as well as retinal screening for eligible members with diabetes, at a $20 copay. Limitations and
coordination with medical coverage may apply.
• Retinal screening for non-diabetic members is covered on an as-needed basis aer a $39 copay.
• Visually necessary contact lenses are covered 100% aer a $25 copay upon review and authorization by VSP.
• Progressive, polycarbonate, tinted and photochromic lenses, as well as anti-reflective or scratch-resistant coatings
and other lens enhancements, will generally receive a 20-25% discount off provider price aer base lens copay.
• Additional discounts for contact lens exams, laser eye surgery, eyeglass frames, sunglass frames and other eligible
items are available.
Additional limits and exclusions apply; see the Insurer Benefits Description for complete coverage details.
No ID card is required. Simply tell your network provider you are a VSP member.
Vision Service Plan | vsp.com | 800.877.7195
WellVision
®
exam
every 12 months
glasses frames
every 24 months
single vision lenses
every 12 months
lined bifocal lenses
every 12 months
lined trifocal lenses
every 12 months
lenticular lenses
every 12 months
contact lens
every 12 months
$15
copay
up to $130
frame allowance
$25
copay
$25
copay
$25
copay
$25
copay
up to $125
lens/exam allowance
portal.insperity.com 9 866.715.3552

portal.insperity.com
866.715.3552
Rev. 09-01-18 | 70-032
